When Your Child Has a Patent Ductus Arteriosus (PDA)
Your child has been diagnosed with a patent ductus arteriosus (PDA). The ductus arteriosus is a normal structure in a baby's heart before birth. It’s a blood vessel that connects 2 arteries. These are the pulmonary artery and the aorta. The pulmonary artery carries blood from the heart to the lungs. The aorta carries blood from the heart to the body. Before birth, the ductus arteriosus allows blood from the right ventricle to bypass the lungs and go directly to the body. This is because the baby gets oxygen from the mother. The ductus arteriosus normally closes shortly after birth once the baby breathes on its own. It’s called a PDA when it stays open (patent). A PDA can lead to heart and lung function that gets worse over time. But it can be easily treated.
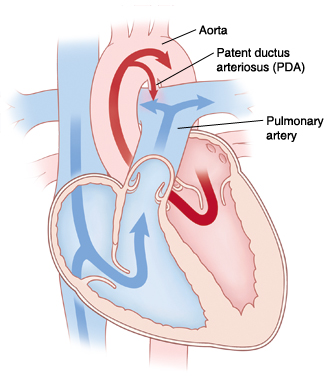 |
| The ductus arteriosus is a normal structure in a baby’s heart before birth. It connects the aorta and the pulmonary artery. If it fails to close after birth, it’s called a PDA. |
Why is a PDA a problem?
With a PDA, blood flows from the aorta through the PDA into the pulmonary artery. This causes increased blood flow to the lungs. If the PDA is large, too much blood goes to the lungs and recirculates to the left ventricle. This can cause fluid buildup in the lungs (pulmonary edema) and enlargement of the left side of the heart. Then the baby has a hard time breathing and feeding.
In severe cases, the increased blood flow to the lungs and overwork of the left ventricle can lead to congestive heart failure (CHF). This is a condition in which the heart no longer pumps blood well.
What are the symptoms of a patent ductus arteriosus?
Most children with a small PDA have no symptoms. Children with a large PDA are more likely to have symptoms. These can include:
-
Trouble breathing or rapid breathing
-
Trouble feeding
-
Slow weight gain
-
Infection of the small intestine (necrotizing enterocolitis)
-
Frequent respiratory infections
-
Heart murmur
How is a patent ductus arteriosus diagnosed?
Heart problems in children are most often diagnosed and treated by a pediatric cardiologist. This is a doctor with extra training to diagnose and treat heart problems in children. The pediatric cardiologist will check your child for signs of a heart problem during a physical exam. To confirm a diagnosis or learn more about a possible heart problem, your child may have several tests. These include:
-
Chest X-ray. X-rays are used to take a picture of the heart and lungs.
-
Electrocardiogram (ECG). This test records the electrical activity of the heart.
-
Echocardiogram. Sound waves are used to create a picture of the heart and look for structural defects and other problems.
How is a patent ductus arteriosus treated?
A PDA may close on its own, without treatment. If it doesn’t, treatment choices are medicine, cardiac catheterization, or surgery. Your child’s cardiologist will assess your child’s heart and talk with you about the best treatment choice.
-
Medicine. Medicine may be the first treatment choice for premature babies. These medicines are usually given by IV. The medicines most often used are indomethacin or ibuprofen. Sometimes multiple doses of medicine are needed.
-
Cardiac catheterization. A thin, flexible tube (catheter) is put into a blood vessel. It’s used to guide a coil or closing device into the heart to close the PDA. The catheter is removed when the coil or device is in place.
-
Surgery. The surgeon will make an incision through the chest on the left side between the ribs (thoracotomy) to reach the PDA. The PDA is clipped or tied off. It may or may not be divided. If it’s divided, the open ends are closed with stitches (sutures).
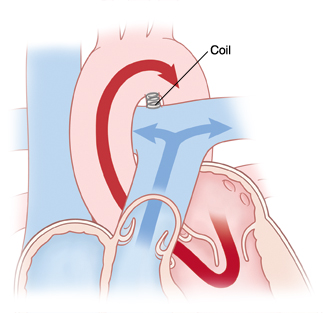 |
| A PDA can be closed with a coil using a cardiac catheterization procedure. |
Risks and possible complications of surgery or cardiac catheterization
Risks and possible complications include:
-
Reaction to contrast dye (with cardiac catheterization)
-
Reaction to sedative or anesthesia
-
Incomplete closure of the PDA
-
Infection
-
Bleeding
-
Abnormal heart rhythm (arrhythmia)
-
Injury to the heart or a blood vessel
-
Injury to nerves
When to call the healthcare provider
Call the healthcare provider right away if your child has any of these:
-
Redness, fluid leaking, swelling, or bleeding at the incision or insertion site that gets worse
-
Fever 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Trouble feeding
-
Tiredness
-
Fast or irregular breathing
-
Cough that won’t go away
-
Prolonged nausea or vomiting
-
Poor feeding or failure to gain weight
Call 911
Call 911 if your child has any of these:
What are the long-term concerns?
-
After repair of a PDA, symptoms related to the defect should go away. Your child should have a heart that works normally.
-
Your child may need follow-up visits with the healthcare provider for 6 months after treatment.
-
Your child may need to take antibiotics for about 6 months before having any surgery or dental work after PDA closure. This is to prevent infection of the inside lining of the heart or valves. This infection is called infective endocarditis. Antibiotics should be taken as directed by the cardiologist.